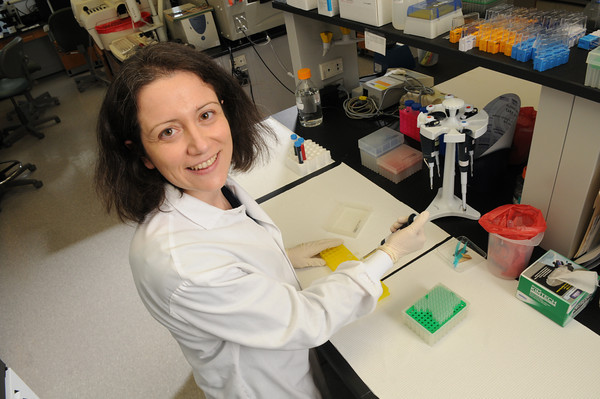
 Alessandra Luchini, a Ph.D. and assistant professor at George Mason University, has helped to invent a “nanoparticle trap” which allows scientists to detect unhealthy cells much sooner than before. When found early, cancer and other diseases are easier to treat, giving patients a better chance for survival.
Alessandra Luchini, a Ph.D. and assistant professor at George Mason University, has helped to invent a “nanoparticle trap” which allows scientists to detect unhealthy cells much sooner than before. When found early, cancer and other diseases are easier to treat, giving patients a better chance for survival.
Recently, Luchini gave a lecture on Nanotechnology in Biomedicine as part of Mason’s Vision Series at the Hylton Performing Arts Center in Manassas, Virginia.
Arriving in the U.S. 10 years ago from The University of Padova in Italy, for a one-year exchange program, Luchini ended up staying on at Mason’s campus in Manassas. There, she works at GMU’s School of Systems Biology and its Center for Applied Proteomics and molecular Medicine and was named one of the “Brilliant 10” young scientists by Popular Science magazine in 2011.
During her Vision Series lecture, Luchini said that even very small tumors or infection sites shed biomarkers into the bloodstream. Biomarkers are unique protein molecules that tell scientists something is going wrong inside the body.
Tiny tumors go undetected
Although scientists have now identified more than 150,000 biomarkers for different diseases, Luchini said, these molecules are very hard to detect in low concentrations. So when a tumor is still tiny, it doesn’t give off enough biomarkers to be found in a patient’s urine or blood stream.
The machines used to detect biomarkers, called mass spectrometers, would need to be improved 100-fold in order to find the miniscule amounts given off by early stage tumors, Luchini said. Making the task even more difficult, the moment that the biomarkers are removed from the body, as part of a blood or urine sample, they begin to degrade, and are quickly lost.
To solve this problem, Luchini and her colleagues came up with the idea of using “smart” nanoparticle traps, consisting of porous soft-shelled polymer spheres smaller than a micrometer across.
They designed the spheres with chemical “bait” molecules inside, which attract and hook the biomarker molecules, trapping them in the shell.
Multi-colored bait
The scientists decided to use dye molecules as bait, because they bind quickly to proteins and hold on to them for hours. Different colored dye molecules trap and hold different biomarkers.
The nanoparticle traps perform several jobs in a single step. First, their shells act as molecular sieves, keeping out larger and more common proteins found in the blood.
At the same time, the particles concentrate the biomarkers into a smaller volume and protect them from degrading.
Once the biomarkers are trapped inside, the nanoparticles are easy to separate out from the blood or urine. Then the biomarkers can be extracted from the traps into a much smaller volume. By concentrating the biomarkers in this way, standard laboratory equipment can now measure how much, if any, there is.
Early detection improves lives
“This technology makes it possible to detect disease that was previously undetectable,” Luchini said.
During her lecture, she presented case studies of three patients who could have benefited from nanotrap technology. These patients were suffering from lung cancer, Lyme disease and Chagas disease, a bacterial infection spread by insects to humans and from mother to child.
In each case, detecting the disease sooner would have made an enormous positive impact on the patient’s life.
Luchini and her team also tested blood taken 25 years ago for a long-range Harvard clinical trial.
Predicting cancer before it starts?
The team found that their nanoparticle traps allowed biomarkers to be detected in patients who years later developed lung cancer, in essence predicting a future illness. This technology may someday help scientists invent a vaccine to block cancer before it starts.
But getting the nanotrap technology into the hands of doctors everywhere will take time.
The Mason researchers are participating in a technology transfer program through Ceres Nanosciences, a company that was spun off from the university to develop commercial applications along with companies like Shimadzu.
The first commercially available test kit using Mason’s smart nanoparticles technology will probably be a urine test for Lyme disease.
So far, this technology has undergone an “all-comers” clinical trial for Lyme disease, which was just completed, and a second regulatory compliance milestone should be finished this summer.
Plans for 2015 include extending the test to detect more strains of Lyme disease.
This article first appeared in the Northern Virginia Times.